More Than Skin Deep – Surviving Melanoma
Season 28 Episode 17 | 26m 56sVideo has Closed Captions
Discover how immunotherapy drugs have changed the way melanoma is treated.
When it comes to skin cancer, melanoma is the deadliest. At one time, it was primarily diagnosed in adults over the age of 50. Today, doctors are seeing an increase in younger people, particularly women, who are facing success with new treatments. See how immunotherapy drugs have made surviving late stages of the disease much more possible. Episode sponsored by UC Davis Health.
Problems playing video? | Closed Captioning Feedback
Problems playing video? | Closed Captioning Feedback
ViewFinder is a local public television program presented by KVIE
Series sponsored by SAFE Credit Union. Episode sponsored by UC Davis Health.

More Than Skin Deep – Surviving Melanoma
Season 28 Episode 17 | 26m 56sVideo has Closed Captions
When it comes to skin cancer, melanoma is the deadliest. At one time, it was primarily diagnosed in adults over the age of 50. Today, doctors are seeing an increase in younger people, particularly women, who are facing success with new treatments. See how immunotherapy drugs have made surviving late stages of the disease much more possible. Episode sponsored by UC Davis Health.
Problems playing video? | Closed Captioning Feedback
How to Watch ViewFinder
ViewFinder is available to stream on pbs.org and the free PBS App, available on iPhone, Apple TV, Android TV, Android smartphones, Amazon Fire TV, Amazon Fire Tablet, Roku, Samsung Smart TV, and Vizio.
Providing Support for PBS.org
Learn Moreabout PBS online sponsorshipMore from This Collection
Programs sponsored by UC Davis Health as part of KVIE’s Focus on Heath initiative.
Video has Closed Captions
Explore deafness and hearing loss through many different lenses. (26m 46s)
Video has Closed Captions
Discover the ways we’ve stayed healthy in mind and body during the pandemic. (25m 29s)
Healing From Home – Telehealth
Video has Closed Captions
Take a look at telehealth today and how modern medicine embraces technology. (26m 46s)
Video has Closed Captions
Meet three resilient individuals facing vision loss. (26m 46s)
Food for Thought – Food Allergies
Video has Closed Captions
Discover the impacts of the food allergy epidemic and what caused it. (26m 52s)
Beyond the Ice Bucket Challenge - Battling ALS
Video has Closed Captions
Discover how early diagnosis and new research changing the lives of people battling ALS. (26m 52s)
Video has Closed Captions
Discover new ways baby boomers are sustaining their health and well-being. (26m 52s)
Video has Closed Captions
Examine the risks of falling and discover measures seniors can take to improve balance. (26m 46s)
The Boomer’s Guide to Growing Older
Video has Closed Captions
Baby boomers are facing ever-increasing challenges. (26m 51s)
Video has Closed Captions
Explore how music and touch become powerful methods of healing. (26m 51s)
Oh, My Aching Back! Prevention & Treatment
Video has Closed Captions
Examine the prevention, management, and relief of back and neck pain. (26m 43s)
The Journey Ahead - End of Life
Video has Closed Captions
Courageous people share their personal stories of end-of-life decisions. (26m 52s)
Providing Support for PBS.org
Learn Moreabout PBS online sponsorship♪♪ Annc: This Viewfinder episode is supported by UC Davis Health, where doctors, nurses, and researchers share a passion for advancing health.
Learn more about their latest medical innovations at health.ucdavis.edu.
Narrator: It'’s the fifth most common type of cancer and the second most common cancer in women under 30.
It'’s curable when caught early, but if not, it can be deadly.
Sometimes, it shows no signs at all.
Dr. Kiuru: Most melanomas are on the skin, but a small percentage can occur elsewhere.
Narrator: The leading cause of melanoma is something we'’re all exposed to, sometimes, most directly in childhood.
Something that defined and delighted many of us throughout our early years.
Dr. Daud: Oftentimes, it'’s sun exposure 20 years, 30 years before you actually get the melanoma.
Narrator: While melanoma isn'’t the most common type of skin cancer, it is the most deadly.
Dr. Gaskill: Because of melanoma'’s ability to leave its primary site and metastasize throughout the body, it is actually the most dangerous of skin cancers.
Narrator: Experts agree that overall incidents of melanoma are increasing.
But so is the survivability, thanks to new therapies.
Dr. Algazi: There'’s a substantial proportion of patients who will live a full lifespan with melanoma and other cancers because of new developments.
Narrator: We'’ll meet one man who developed stage four melanoma in adulthood, just as immunotherapy treatments were becoming available.
Mike Gaynes: If it had happened six months earlier that I had gone to stage four, I likely would not have survived.
Narrator: And we'’ll explore the story of a young woman who has been diagnosed with melanoma twice.
Kelsey Cowin: When they first diagnosed, I was like, "Okay, what is my life going to look like?"
Narrator: We'’ll also discover a new kind of treatment for melanoma that'’s changing how this cancer is handled, and increasing the chances of survival.
Dr. Algazi: We can harness the immune system to help fight cancer and keep patients well for a long time, possibly indefinitely.
This is More Than Skin Deep: Surviving Melanoma.
>>: Hello.
>: Hello.
>>: How are you doing today?
>: Good.
How are you?
>>: Good.
Everything going okay?
>: Yep.
Kelsey Cowin: I was diagnosed with stage three melanoma in April of this year and I'm going to have surgery for it in- on Friday.
Narrator: While most new melanoma cases today are found in people over the age of 50, 31-year-old Kelsey Cowin is part of a growing number of women between 15 and 30 years old who are being diagnosed with advanced stage melanoma.
What may surprise you even more- this isn'’t her first time.
Kelsey: So, I was originally diagnosed with melanoma in, um, 2012 when I was 22.
Narrator: Kelsey has been a regular sunscreen applier her whole life and has seen the dermatologist twice a year since age 14.
Her grandfather had another form of skin cancer, and her mother was later diagnosed with melanoma as well.
She'’s among an estimated 10% of melanoma patients whose cancer has genetic origins.
So, she was taught to pay close attention to her skin health at an early age.
In fact, she'’s the one who noticed a suspicious mole on her forehead.
Kelsey: I was like, "“Okay, that looks strange.
I need to go get that looked at.
"” And it turned out to be melanoma.
Narrator: The first time Kelsey was diagnosed with melanoma, it was handled the same way it would be now- with surgery to remove the cancer and determine if it spread to other parts of the body.
She was in her senior year of college at Cal Poly San Luis Obispo at the time and just wanted a normal, healthy college life.
She had that surgery and then returned to campus, relying on her roommates to help her through the hard days, and make life feel normal again.
Kelsey: So, they would help me change my bandage, and then I'd, like, put a little headband over it so nobody could see it and just go to school like normal.
Narrator: Fortunately, the surgery was successful.
There was no sign the melanoma had spread.
Kelsey was able to bypass chemotherapy which, at the time, would have been the next step- a physically and emotionally challenging next step.
She stayed at Cal Poly and graduated in 2012.
Ever since, Kelsey has had regular monitoring and skin checks every three months, which is probably why she was aware enough to discover the cancer for a second time, nearly a decade later.
Kelsey: To have melanoma was definitely shocking, and then, to have it re-diagnosed nine years later was even more shocking.
So- Narrator: This time, the melanoma appeared as a lump on her neck.
It had spread to her lymph nodes.
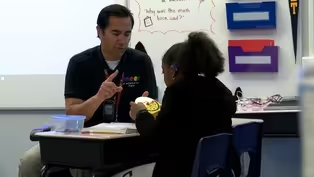
Dr. Gaskill: What I'’m focused on in the middle here is your SCM.
Narrator: Kelsey is here at UC Davis Cancer Center for a final appointment before her surgery to remove the melanoma.
Kelsey: They are taking out my Parotid gland, which is the gland that my, uh, tumor is in.
Dr. Gaskill: You can see this node right here that lights up.
That's the area of disease that she was diagnosed with, the recurrence.
Narrator: Kelsey'’s doctor is Cameron Gaskill, a surgical oncologist at UC Davis Health.
Dr. Gaskill: So, Kelsey's a, uh, interesting case.
Narrator: "“Interesting"” because she was technically in remission for years before being diagnosed the second time.
Most melanoma re-occurrences happen within five years of the initial discovery and if a patient remains melanoma-free for ten years, it'’s far less likely the cancer will return, but not impossible.
Also, there are treatments available now that didn'’t exist before.
Dr. Gaskill: What's exciting about her case is that we're offering her an immunotherapy that was just becoming available- just, the studies were just being done 10 years ago, when she had her initial diagnosis.
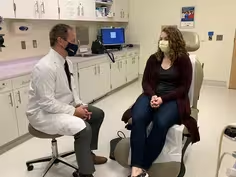
Narrator: But today, the focus is on her surgery, where Doctor Gaskill explains, there'’s no room for error.
>>: ... sore neck and cheek.
>: Yes.
Hopefully not too bad.
Dr. Gaskill: Right now, what we have is a... a lymph node with evidence of metastatic disease.
And that lymph node is right on the parotid gland, which helps to produce saliva for your mouth.
Unfortunately, you know, the... the anatomy is such that, uh, the nerve that controls a lot of your facial function goes right through the parotid gland.
That'’s it.
So, we'’re going to take that out with the surrounding parotid gland around it.
To treat this disease, we'’ll need to take the first part of the parotid gland as well as all of the lymph nodes in that side of the neck.
Narrator: Because there are several important nerves that go through the parotid gland, he'’s put together a team of experts that include head and neck surgeons, a radiation oncologist, and other specialists.
Four days after this visit with Kelsey, Doctor Gaskill sees her again.
This time, in the operating room, along with the team he has assembled for a very technical surgery.
Dr. Gaskill: It's a, uh, invasive procedure where we're, uh, operating around a lot of important vessels and nerves and needing to preserve their function while still getting all of the lymphatics and lymph node tissue out so that, uh, we leave no cancer behind.
Narrator: Ten years ago, any detection of melanoma in the lymph nodes would almost certainly require the surgery to be followed by chemotherapy, essentially a poison designed to attack the cancer.
It'’s often incredibly hard on the body.
Chemo was the standard of care, until recently.
Now, doctors turn to immunotherapy to treat patients with stage three or four melanoma.
Immunotherapy works differently.
It'’s designed to fire up the body'’s immune system to kill the cancer itself.
Dr. Daud: In the last 10 years, I think people- you know, there's just so much more information on how the immune system works.
Narrator: Doctor Adil Daud is an immunotherapy researcher at UC San Francisco and co-founder of the melanoma center there.
He helped develop some of the life-saving immunotherapy drugs that are widely used today to fight melanoma and other immunogenic cancers.
Some cancers, like melanoma, are known to be highly immunogenic, which means the body'’s t-cells- the working end of the immune system- can mount their own response to the cancer cells.
Dr. Daud: In many cases, your immune system already recognizes cancers and already starts to attack them.
Narrator: Immunotherapy just gives those t-cells a big boost, amplifying an immune reaction that'’s already happening, and changing outcomes for many patients.
Dr. Daud: If the melanoma responds well to immune therapy, you could be alive for many, many years.
Narrator: Dr. Daud says chemotherapy drugs just didn'’t work as well with melanoma.
In 2000, if you were diagnosed with advanced stage melanoma, doctors say you may have lived another six to nine months.
There were other treatments that worked- like B-RAF inhibitors- but doctors found that after about a year, patients often developed resistance to them.
Today, with immunotherapy, there'’s a 65% chance you'’ll live five years or longer.
Dr. Daud: I think, when it became clear to us that immunotherapy was the... was the best approach for most patients with melanoma is when we started looking at some of the survival curves of patients who were treated.
Narrator: Immunotherapy has become the go-to treatment for anyone diagnosed with advanced stage melanoma.
It'’s proving to be much easier for patients to handle, and much better for doctors who have to deliver the news.
Dr. Daud: I remember the time when I was worried about looking at people straight in the eye and say, "“Yeah, you know, they'll do this type of treatment and I think it's gonna work for you.
"” Dr. Algazi: I'd say it's miraculous.
It's really exciting.
I mean, if you imagine working for NASA in the sixties, you couldn't imagine something that seemed hard to do- Like Kennedy said, "We don't do it because it's easy.
We do it because it's hard."
And then it works.
And then, you see the guy on the moon.
It's like, how exciting is that?
Well, this is, in a sense, almost bigger than this.
Narrator: Immunotherapy has proven so promising and so groundbreaking that in 2018, two medical researchers won the Nobel Prize for it.
In Kelsey'’s case, immunotherapy gives her the best chance at beating this disease.
Doctors often don'’t know the exact odds, but many of the patients who have found success with immunotherapy are still alive.
Dr. Gaskill: The prognosis overall for her, with node positive disease, is in that initial 65% of five-year survival.
But that being said, those are numbers from, you know, the early 2000s, and so, it's tough to say how well those apply to our current patients.
Narrator: Not everyone does respond to immunotherapy.
Between 20 and 30% of patients just don'’t seem to benefit at all.
30 to 40% have partial responses, meaning the cancer shrinks but doesn'’t completely disappear.
For as many as 20%, the disease remains stable, and for 15 to 20% of immunotherapy patients with stage four melanoma, the treatment is followed by a full response.
They go into remission and stay there.
65-year-old Mike Gaynes is one of those patients.
He grew up in an era where sunscreen wasn'’t yet a household item, tanning beds were still on the horizon, and no one outside of the medical community gave much thought to skin health.
Mike Gaynes: It occurred because I spent 40 years playing soccer in the sunshine before they invented sweat-proof sunblock.
Narrator: Around the same time, and for years to come, oncology doctors who specialized in melanoma were knowingly entering a field where most of their patients wouldn'’t survive.
That was the case for UCSF oncologist- and Mike Gaynes'’ doctor- Alain Algazi when he began his career just over a decade ago.
Dr. Algazi: I remember when I first started doing melanoma, we had a relatively small patient panel '‘cause everybody would die within a year.
It was horrible.
Narrator: Melanoma is often deadlier than other more common skin cancers because of the way it invades lymph channels, spreading throughout the body and re-establishing itself in lymph nodes.
For Mike Gaynes, it first appeared in 2013 when he noticed a lump on the side of his neck that turned out to be stage three melanoma.
Mike: It was not shocking to find out that it was cancer.
It was shocking to find out it was melanoma.
Narrator: Mike says it also didn'’t appear on his skin, which is uncommon.
According to doctors, only 2 to 4% of advanced melanoma cases start with unknown primaries.
The cancer was removed, and his scans came back clear.
Mike: I had gotten used to the fact that if the cancer came back, I was in deep trouble.
Narrator: Two years later, the melanoma was back.
This time, in his belly, and this time, it was stage four.
A terrifying diagnosis that, just a few months earlier, might have been interpreted as a death sentence.
But there were new options that had just been approved weeks earlier.
He was among the first at UCSF to be treated with immunotherapy drugs.
Mike: "“A chance to live longer.
"” That's what this was.
He told me straight-out to live as if I had two years.
Narrator: That was six years ago.
While it wasn'’t exactly a walk in the park, Mike Gaynes marvels at the fact that he was still able to play soccer while undergoing immunotherapy treatment.
That'’s him, the goalkeeper.
He says being able to do the things he loves in life, like community theater, even while battling a deadly disease, made him feel more alive, and more grateful than ever before.
Mike: To bang into people and yell at the referees and trip over the ball and holler at somebody for not making the right pass.
You'’re just so alive.
Narrator: The day we interviewed Mike was his 65th birthday.
He celebrates each birthday by going to the gym and bench pressing his weight just to prove that he'’s still strong enough.
Dr. Gaskill: I think the silver lining in this is that we have better therapies, uh, to treat advanced stage melanoma.
So, overall, our survival'’s improving.
Kelsey: As disruptive as cancer is, this drug that I'm on has been great.
Narrator: For Kelsey Cowin, immunotherapy has allowed her to continue working full-time as an environmental consultant and living much the same life she did before.
She even got married this year, all while undergoing the immunotherapy infusions that she started before her surgery.
And Kelsey got some great news following that surgery.
The pathology report showed no active cancer, meaning she has had a full response to the immunotherapy.
Kelsey: Well, the option to not have to use chemotherapy, to be able to use immunotherapy, the- Just, my lifestyle, in general, hasn't really changed, you know, since I have been diagnosed.
Narrator: At this visit, she'’s accompanied by her college friend, Carrie, who helped her through her first fight with melanoma.
This time, she'’s walking with Kelsey through an experience that'’s much more tolerable than it would have been just a decade ago.
Kelsey: Not having to lose my hair, you know, all of those side effects from chemotherapy just, really, haven't been at play for me.
Narrator: While immunotherapy has made life easier for patients like Kelsey, it has brought a lot of joy to the lives of doctors who have also been battling melanoma- but in a different way- and now know that it'’s very possible for their patients to survive.
Dr. Algazi: You see people who are well, you know, who you would have expected to die.
People have a new lease on life, who can do normal things, and celebrate birthdays, and weddings, and grandchildren, and all of those things.
It's really exciting.
It was one of those things you couldn't conceive of maybe a few years ago.
And that's... that's about as good as it gets.
Narrator: While the treatment may have vastly improved, the danger will always exist.
We can'’t very easily escape the sun, especially in California, which leads the nation in the number of melanoma cases each year.
There are stern warnings now about what sun exposure can do to us, long term, and why it'’s so important to protect ourselves from it.
That goes for tanning beds, too, which now carry regulations in many states to prohibit teens from using them and potentially creating damaging sunburns that could lead to skin cancers.
Dr. Daud: My colleagues here at UCSF have, in the dermatology program, a lot of their effort has been to try to get the legislature to... to at least put warning signs and... and not to allow young people to use tanning beds and tanning salons and stuff like that, because you're basically just creating DNA damage there.
Narrator: California was the first state to ban minors from using tanning beds, in an effort to cut down on skin cancer of all types.
But doctors say they still see a lack of understanding about who can get skin cancer.
Thinking that it can'’t happen to you because it doesn'’t run in your family, or you live in a cloudier region, or you don'’t have the right skin type, is dangerous thinking.
Dr. Daud: That idea that only fair skin people get it is... is incorrect and... and of course, that leads to a lot of delayed diagnosis.
Narrator: According to the American Cancer Society, melanoma doesn'’t discriminate.
While the odds are greater for Caucasians - their overall lifetime risk of getting melanoma is one in 38.
For Hispanics, it'’s one in 167, and one in 1,000 for African Americans.
In short, anyone who is exposed to the sun can get melanoma and, often, those who spend the most time in the sun, are the least likely to be aware of the danger.
Dr. Gaskill: Some of the risk factors are childhood sunburns, childhood blistering sunburns.
Narrator: As for patients like Kelsey, and other young women who are faced with a melanoma diagnosis, researchers are still looking into why they are a higher risk category.
Doctor Maija Kiuru, Associate Professor of Clinical Dermatology and Pathology at UC Davis, studies the connection of melanoma and genetics and says there'’s still much to learn about who melanoma affects, in particular, when it comes to younger women, like Kelsey, who have steered clear of the sun and been smart about exposure.
Dr. Kiuru: There could be other reasons, as well, that we don't fully understand, but, uh, potentially hormonal differences between men and women.
And then, also, differences between the immune systems of men and women.
Narrator: Among their recent discoveries, researchers have also learned the BRCA2 gene- one of the '‘breast cancer genes'’- bears a melanoma connection, but they'’re still learning what that connection is.
The good news- genetic testing can help identify those who might be at a higher risk.
Dr. Kiuru: So, roughly 10% of patients will have somebody else in the family who has melanoma, but a much smaller percentage of those will actually be at a much higher risk and the risk can be determined in each of the family members, um, by genetic testing, in some cases.
Narrator: Doctor Kiuru says, regardless of any familial connection, regardless of your skin type or how much sun exposure you'’ve had, something everyone should be aware of is the "“A-B-C-D-E"”s of skin cancer.
Dr. Kiuru: So '‘A'’ is for asymmetry.
Narrator: Which means if you have a lesion that you cut in half, one side may not look like the other side.
Dr. Kiuru: '‘B'’ is for borders, irregular borders.
Narrator: It may have a scalloped or not well-defined border.
Dr. Kiuru: '‘C'’ is for colors.
So, variable colors.
Narrator: The spot may have shades of tan, brown or black, or even areas with red or blue.
Dr. Kiuru: '‘D'’ is for diameter, larger size.
Narrator: According to the Amercian Academy of Dermatology, melanomas are usually greater than 6 millimeters, or about the size of a pencil eraser when diagnosed, but they can be smaller.
And finally... Dr. Kiuru: '‘E'’ is for evolution.
So, any change over time would be something that we would want to know about.
Narrator: All of the experts will tell you, however, that the best way to protect yourself from melanoma and other skin cancers is to be proactive.
Dr. Gaskill: And so, that means wearing long sleeves, wearing sunhats, wearing sunblock, not going to tanning beds, all those.
Narrator: And while California summers may not lend themselves to long sleeves, these days, it'’s not hard to find products, including clothing, that'’s built for sun protection.
>>: Let me see the back.
Ok!
I think our customers will love this.
Narrator: Rhonda Sparks is the creator of UV Skinz, a sun protection apparel company out of Sonora, California that'’s focused on selling peace of mind- clothing that could literally save your life.
Rhonda Sparks: All of our products are UPF 50+, um, and basically, what that means is that it blocks 98% of UVA and UVB rays from penetrating the fabrics.
So, you won'’t get a sun burn.
Narrator: For Rhonda, this isn'’t just a clothing line.
It'’s a mission born out of the despair of losing someone she loves, and the desire to help others avoid the same kind of pain.
Rhonda: UV Skinz started because I lost my first husband to melanoma.
He was 32 years old and we had 3 little boys at the time of his passing.
They were one, three, and six.
Narrator: After her husband passed away, Rhonda started UV Skinz in a barn on her property as a way to recover and to help fight back against this deadly disease.
Her husband'’s fight with cancer took place before immunotherapy drugs were available.
The options for melanoma patients at the time were few, and the outlook was grim.
Fighting melanoma was truly a battle, one that Rhonda Sparks fought in her own way.
Rhonda: We call our sun protection apparel "“sun protection soldiers.
"” Every unit that leaves our warehouse is on a mission, and that mission is to help save lives.
Narrator: Nordstrom was the first major retailer of UV Skins, which has also been featured on TV shows, like The View and the Today Show.
>>: Yeah.
We got some great, sporty swimwear styles.
To begin, Evan is wearing a great piece by UV Skins.
Narrator: And now, more than two decades later, Rhonda is remarried, her business is more successful than she could have imagined, and most importantly, she finds comfort and purpose in knowing she'’s helping others.
Rhonda: The lessons that I'’ve learned going through the loss of Darren have just been immense.
Your heart breaks into a million pieces from the loss, but then, it literally comes back, I feel like, even bigger because of the compassion I have for people, and the empathy.
Narrator: It may be a similar kind of compassion that doctors feel as they treat patients with advanced cancer and search for ways to make their lives longer and better.
Dr Algazi: When I'm seeing somebody like Mike, I don't want him just to live for another few months.
I want him not to die of cancer, full stop.
You know?
I want him to stay well indefinitely.
Narrator: While doctors do their best to keep patients healthy, they have to rely on patients to do their part, which includes not only protecting their skin, but visiting the dermatologist annually.
Dr Algazi: Keep close tabs on your skin.
The best way to treat melanoma is to not let it grow.
If you have something that's concerning, have your dermatologist take a look at it, go to your primary doctor.
Kelsey: The sooner you find it, the easier it's going to be for you.
The treatment is great when you find it early.
Narrator: Research shows that a stage one melanoma diagnosis comes with a more than 90% chance a patient will be cured.
Those numbers decrease, the later the stage of discovery.
Dr. Algazi: Today, if you walk in with melanoma, I say the chances are better than not that you will survive, even with widely metastatic disease.
Narrator: It'’s an exciting prospect for oncologists facing a future where melanoma may, someday, be more of an inconvenience than a death sentence.
Dr. Gaskill: It feels like we're coming out of the dark ages of... of chemotherapy, where we're able to offer patients specific therapies for their specific cancers, and we see great results from that.
Dr. Algazi: I think we all think that there is a world of possibility in terms of making treatments that will work for more patients, that we could make all of these cancers- head and neck cancer, melanoma, lung cancer- we can make them treatable diseases where the average person, even with widespread disease, doesn'’t die.
Narrator: The hope that other types of cancer patients will someday also benefit resonates with people like Mike Gaynes, who twice survived melanoma and credits this miracle of modern medicine for helping him.
Mike Gaynes: It's a game-changer, from a medical perspective.
From a human perspective, it's a life-changer.
It's a world-changer.
The color of the sky changes, just because you have a hope where there might not have been one before.
Not just the hope of survival, but a hope of survival with a really good quality of life.
Narrator: It'’s a battle that'’s More Than Skin Deep: Surviving Melanoma.
Annc: This Viewfinder episode is supported by UC Davis Health, where doctors, nurses, and researchers share a passion for advancing health.
Learn more about their latest medical innovations at health.ucdavis.edu.
More Than Skin Deep – Surviving Melanoma Preview
Preview: S28 Ep17 | 30s | Discover how immunotherapy drugs have changed the way melanoma is treated. (30s)
Providing Support for PBS.org
Learn Moreabout PBS online sponsorshipSupport for PBS provided by:
ViewFinder is a local public television program presented by KVIE
Series sponsored by SAFE Credit Union. Episode sponsored by UC Davis Health.