Food for Thought – Food Allergies
Season 25 Episode 12 | 26m 52sVideo has Closed Captions
Discover the impacts of the food allergy epidemic and what caused it.
Discover the impacts of the food allergy epidemic and what caused it.
Problems playing video? | Closed Captioning Feedback
Problems playing video? | Closed Captioning Feedback
ViewFinder is a local public television program presented by KVIE
Series sponsored by SAFE Credit Union. Episode sponsored by UC Davis Health.

Food for Thought – Food Allergies
Season 25 Episode 12 | 26m 52sVideo has Closed Captions
Discover the impacts of the food allergy epidemic and what caused it.
Problems playing video? | Closed Captioning Feedback
How to Watch ViewFinder
ViewFinder is available to stream on pbs.org and the free PBS App, available on iPhone, Apple TV, Android TV, Android smartphones, Amazon Fire TV, Amazon Fire Tablet, Roku, Samsung Smart TV, and Vizio.
Providing Support for PBS.org
Learn Moreabout PBS online sponsorshipMore from This Collection
Programs sponsored by UC Davis Health as part of KVIE’s Focus on Heath initiative.
Video has Closed Captions
Explore deafness and hearing loss through many different lenses. (26m 46s)
More Than Skin Deep – Surviving Melanoma
Video has Closed Captions
Discover how immunotherapy drugs have changed the way melanoma is treated. (26m 56s)
Video has Closed Captions
Discover the ways we’ve stayed healthy in mind and body during the pandemic. (25m 29s)
Healing From Home – Telehealth
Video has Closed Captions
Take a look at telehealth today and how modern medicine embraces technology. (26m 46s)
Video has Closed Captions
Meet three resilient individuals facing vision loss. (26m 46s)
Beyond the Ice Bucket Challenge - Battling ALS
Video has Closed Captions
Discover how early diagnosis and new research changing the lives of people battling ALS. (26m 52s)
Video has Closed Captions
Discover new ways baby boomers are sustaining their health and well-being. (26m 52s)
Video has Closed Captions
Examine the risks of falling and discover measures seniors can take to improve balance. (26m 46s)
The Boomer’s Guide to Growing Older
Video has Closed Captions
Baby boomers are facing ever-increasing challenges. (26m 51s)
Video has Closed Captions
Explore how music and touch become powerful methods of healing. (26m 51s)
Oh, My Aching Back! Prevention & Treatment
Video has Closed Captions
Examine the prevention, management, and relief of back and neck pain. (26m 43s)
The Journey Ahead - End of Life
Video has Closed Captions
Courageous people share their personal stories of end-of-life decisions. (26m 52s)
Providing Support for PBS.org
Learn Moreabout PBS online sponsorship♪♪ Announcer: This ViewFinder episode is supported by UC Davis Health, where doctors, nurses, and researchers share a passion for advancing health.
Learn more about their latest medical innovations at health.ucdavis.edu.
♪♪ ♪♪ NARRATOR: Food allergies, 50 years ago, they were almost unheard of.
Now they're an epidemic.
I'm allergic to peanut, tree nuts, shellfish, and fish.
One in 10 children have some kind of serious food allergies.
This is a scientifically defined epidemic.
NARRATOR: Nut allergies have more than tripled in kids in the past 14 years.
This immunotherapy, you don't have to be so worried about these foods anymore that can possibly kill you.
NARRATOR: The Giorgis 13-year-old Natalie was allergic to peanuts.
She was sick and then was struggling to breathe.
NARRATOR: Natalie's identical twin sister, Danielle, has the exact same peanut allergy.
Tragically, Natalie died from an accidental exposure to peanuts.
I tell people all the time, she looked exactly the same way in this life that she did in death.
Unfortunately, sometimes changes come about because they're written in blood.
♪♪ Narrator: Food for Thought.
What you need to know about food allergies.
Joanne Giorgi: What are you doing, Natalie?
Natalie, what are you doing?
Flying my kite!
♪♪ Narrator: The Giorgi family lived in Carmichael, California, among the trees, great neighbors, near parks and good schools.
Joanne: We loved our time we were in Sacramento for 10 years.
Narrator: Many summers, the Giorgi family traveled from Carmichael up to the mountains of the Sierra Nevada, vacationing at Camp Sacramento.
Joanne: It was our last night at camp.
There were some snacks out, and Natalie took a bite from a Rice Krispie treat that unknowingly had peanut butter in it.
Narrator: That night in July 2013, something went horribly wrong.
...17... My birthday's in 18 days.
Narrator: From the time they were little girls, the Giorgis twin daughters had been identified as being allergic to peanuts and tree nuts.
Joanne: The kids always used to identify themselves when they'd get there.
They'd say, I've got the nut allergy, and so we kind of had a system when they'd go through the food line.
Narrator: The 13-year-old twins had allergy action plans that included epi pens in case of an accidental exposure.
Louis Giorgi: We had been at this camp and had the same Rice Krispie treats many times, so she took the bite.
Joanne: And she came to us and said, I don't know what the Rice Krispie treat had, but I don't know if it maybe had peanut butter in it.
We followed her allergy action plan and we gave her a Benadryl and she had no symptoms.
Narrator: Then Natalie went into anaphylactic shock, a life-threatening allergic reaction that causes the immune system to release a flood of chemicals.
Her blood pressure dropped.
Breathing became difficult.
Louis: We gave her the medicine and got her into the nurses' station.
Narrator: Natalie's dad, Louis Giorgi, is a doctor.
Louis gave her the first of three shots of epi.
Narrator: He smashed his elbow through a glass medicine cabinet to grab yet another epi pen.
Joanne: Her airway was closing off.
Narrator: Natalie did not have swelling or hives.
They're often expected during a reaction.
Joanne: People need to understand that it's not some sort of idea of swelling, and while it can be, it can also be silently doing something to the sufferer on the inside.
Narrator: An ambulance and Life Flight arrived in the mountains near Camp Sacramento.
But it was too late.
Louis: I'm sure she, I'm sure she was gone on the hill.
Danielle Giorgi: I knew that something was wrong before I was even told.
Probably, I don't know, twin telepathy or something, but I just knew something was off, and I could kinda feel it.
Michael Giorgi: Everybody in my family has suffered with the fact, like survivor's guilt, like the pain of just being there.
Travis Miller: I saw Natalie as a patient when she was much younger, her and Danielle, single digits, seven or eight years old.
They had food allergy and asthma.
Like any other-- Childhood death, there's no words.
There's nothing I could ever say.
I believe sort of more in the power of a really prolonged hug and sharing tears.
Narrator: Looking for accountability, the Giorgis filed a lawsuit against the City of Sacramento.
Louis: Camp Sacramento did take responsibility for it and has made changes now to keep others safe.
The lawsuit was a step we took as part of the mission, part of the goal of raising awareness.
It is a tool that helps people pay attention.
It was important for us because Natalie just didn't disappear.
Natalie mattered, and all these kids matter.
She did nothing wrong, and we did nothing wrong, and our kids and people need to know that, as well.
Narrator: The lawsuit has raised awareness about food allergies.
It's also made camp cafeterias across the country much safer for people with food allergies.
Louis: If we had known what was in there, she wouldn't have eaten it and we wouldn't be interviewing, wouldn't be talking to you right now.
Michael: Mom, do I have baseball this weekend?
Joanne: No, baseball has been canceled.
Narrator: As difficult as it is, life must go on.
Joanne: Natalie and Danielle are our oldest.
We have a daughter Catherine and a son Michael.
Narrator: Food allergies often are genetic.
Catherine and Michael have been tested and are negative.
Michael: Honestly, I wish nobody would have it and I just kinda want it to go away.
So I think you're kind of like, it's the right thing to do to go and tell people about it, so this issue can change.
Catherine Giorgi: At first, I was scared because I thought there's no way I wasn't allergic (laughs), but I wasn't.
Narrator: Dairy is the most prevalent food allergy.
Peanuts are second.
Travis: Interestingly, dairy, cow's milk, eggs, wheat, and soy are the food allergies that children tend to outgrow more frequently, especially by the time a child is five or six years old.
Victoria Dimitriades: We tend to think of nuts and shellfish, seafood to be the most salient allergy, so you're much less likely to outgrow those foods, maybe 10 to 20% chance, whereas in terms of milk or eggs, you're much more likely to outgrow those food allergies, and that can be up to 80% of patients.
Narrator: Fewer people outgrow their peanut and tree nut allergies, and that's why we hear about them more.
Peanuts, by the way, are legumes, but they contain proteins similar to those found in tree nuts.
Tree nuts include almonds, Brazil nuts, walnuts, hazelnuts, macadamia nuts, pistachios, pecans, and cashews.
Travis: If you have food allergy, you're much more likely to have another type of allergy.
Narrator: Again, Natalie was allergic to nuts but also had asthma.
So does her twin sister, Danielle.
Joanne: Danielle has started with an injection of a medication that they put her on after Natalie's passing, something called XOLAIR, and so Danielle gets an injection of that.
Travis: Her asthma got better.
Her ability to feel safe increased.
Her parents' anxiety was decreased.
Narrator: XOLAIR is an asthma medication that's proving to be effective for food allergies.
If we're treating using XOLAIR for protection of food allergy, it's currently off-label.
Narrator: That means it's not yet FDA approved for treatment of food allergies, but it's being fast tracked.
Travis: There is an accumulating body of data showing that using XOLAIR can decrease the intensity of reactions, the severity of reactions, can decrease the frequency of reactions.
Rubina Inamdar: If you talk to our elders, our grandparents, they don't remember children having food allergies.
When you go from one in 100 to one in 10, it's definitely an epidemic.
Narrator: 14-year-old Michael Lee is Sacramento's patient zero for a new protocol called oral immunotherapy or OIT.
He's allergic to peanuts and tree nuts.
Joanne: I think all of these young people are courageous who go through the OIT or whatever trial they are part of and whatever therapies they're looking for, because they are the ones who are helping us get closer to a cure.
Travis: Every anniversary that goes by, every birthday, every holiday, the anniversary of Natalie's passing is a reminder, so there's an extra layer of intensity that I think the Giorgi family deals with.
So oral immunotherapy may not be part of Danielle's long-term treatment program.
Narrator: OIT is a rigorous program.
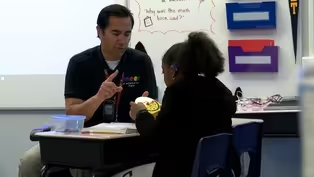
Dignity Health's Dr. Rubina Inamdar and Michael are pioneering the way.
"(laughs) And how about" "those other tree nuts--" Michael Lee: First reaction I had was when I was four years old in kindergarten.
I was fed a pretzel laced with peanuts and it gave me a reaction immediately.
The symptoms include hives, itching in the mouth, and sometimes in severe situations, anaphylactic shock, which really troubles my breathing and usually requires a visit to the ER.
Narrator: After learning that Stanford was doing oral immunotherapy, Michael's mom, Geena Lee, wanted the groundbreaking treatment for her son.
That was five years ago.
Geena Lee: That's when I found Dr. Inamdar and I told her about this immunotherapy that was developed at Stanford, and I mean, she was very gracious, but more apologetic about the fact that that was not available at the time.
I thought, well, I'm just stuck with an epi pen and paranoia for the rest of my life and his life.
Narrator: An epi pen is an injection of the drug epinephrine and a life-saving medication for treating food allergy reactions.
But why all of these food allergies now?
Hand sanitizers may be part of the answer.
Travis: Hygiene hypothesis has been around for close to 20 years now.
We thought it may be most of the answer, and in reality, I think we think it's part of the answer.
Rubina: There's definitely data on antibiotic use changing the way our gut interacts with food, and the second thing is the way we as a community interacts with food.
Travis: American Academy of Pediatrics in the late '90s came out with recommendations to avoid high risk foods-- Then the goal ultimately-- Based on scant data.
Rubina: Because there was a few cases of people developing peanut allergy, we all told people not to eat peanuts for a long time, and now we've given that allergy to many more people.
And so our job is to try to reverse that trend as best as we can.
Victoria: Children that are introduced many different types of foods at an early age are less likely to develop allergies overall, both food allergy and environmental allergy.
Narrator: After the call from Michael's mom about OIT, Dr. Inamdar began researching clinical trials.
Geena: She calls me and says, well, you know, guess what?
I was able to get this immunotherapy at our hospital.
And I said, that's great, when can I come in?
(laughs) That was my next word, and she goes, well, I would like to invite your son to be patient zero.
Rubina: And what we do is we find out that somebody has a peanut allergy and we start giving them very, very tiny amounts of this food, a little bit, a little bit, a little bit at a time.
We get their body used to it.
It's old style medicine.
We can get somebody eating peanuts within a matter of a few months.
Narrator: Michael's OIT was started in the allergist's office under close supervision.
The first time, he went into anaphylaxis.
Rubina: We followed the directions according to what we understood to be the directions, and on the final dose, Michael had a reaction.
Michael: I started having an immediate reaction.
My throat started getting tingly.
I started feeling terrible.
Geena: The doctor was there, the nurses were there.
They immediately came through.
When they saw the onset of symptoms, they came and treated it right away.
Epi pens, definitely monitoring his situation.
They'd never tried it up here.
Narrator: People with food allergies are also prone to a skin condition called eczema.
It's a lot to manage.
Geena: Currently what I'm doing is measuring nuts.
It started with peanuts, but I'm measuring peanuts and walnuts and cashews and almonds.
I mean, he's eating the very thing that he's allergic to.
Narrator: When Michael's asthma flares up, his food allergies get worse.
His doses must then be cut back.
Michael's mother carefully weighs, measures, and administers doses of nuts to her son.
Geena: He'd have to take it every 12 hours, so I'd have to count every 12 hours.
I set an alarm for everyone, my husband, myself, alarm every 12 hours.
We would be at an amusement park.
12 hours, they'd have to stop, not go on the ride, and you'd have to eat your peanuts, and it was very strict.
Michael, did you eat your nuts today?
Michael Lee: Not yet.
Come on.
I guess, I will now.
Michael: It's scary because you know your life's on the line when you have something that bad like a peanut, so I just think that this immunotherapy is just helping so much to mediate that stress and that worry that eating a peanut, Good job, man.
MICHAEL LEE: or just something simple like that would threaten your life.
Thanks.
Rubina: There's no reason for little children born in the last couple of years to be developing peanut allergies unless somebody isn't paying attention.
Narrator: Michael still carries an epi pen at all times, but the hope is he'll never need it again.
Michael: It's turned out so well for me.
Peanuts earlier, just a little bit of it would trigger a huge reaction, and now, Reese's Peanut Butter Cup, it's fine.
Five grams of peanuts, fine.
Peanut butter, it's fine.
So much worry is gone just by this therapy.
♪♪ Narrator: Because genetics play a big role in allergies, Michael's brother has been tested.
He's lucky, no food allergies.
Michael Lee: My brother, his name's Robert Lee.
Occasionally, we play duets together to perform for other people.
Narrator: Five years of immunotherapy and Michael's experiencing a newfound freedom.
It's almost as if he's sailed somewhere over the rainbow.
Victoria: What we know is that there is a lot of potential for children to develop food allergy, but with some mild interventions, we are able to impact that in the future.
"Hello, there, good morning."
Narrator: Treating high risk children at an early age is critical in ending this epidemic.
"Are you gonna wake up?"
Travis: Garrett's five months old and his mother is highly allergic.
She has severe asthma, food allergies, environmental allergies, medication allergies.
She's had multiple anaphylactic reactions herself to a variety of different things.
She actually receives XOLAIR as part of her treatment.
LaRetta Semilla: Being allergic puts him at a higher risk.
Along with my husband, he has severe eczema and Garrett's already shown the signs of eczema.
Narrator: Garrett is being allergy tested to assure it's safe for him to undergo a new allergy treatment protocol.
Travis: We only have to do limited skin testing, and then, since he's five months old, he's in that window of early introduction.
We wanna do a, it's called a Bamba challenge.
Bamba is a baked peanut puff, (Garrett cries) so it has lower amounts of peanut protein.
We're looking for three and four, and he's actually gonna land over there, which is good.
That means that (baby shrieks) we can proceed.
Oh, oh, oh.
Narrator: The Bamba snacks are cut into small pieces and mixed with water.
Travis: I like the Bamba challenge because-- "Yum!"
She's been feeding a rice cereal which is very similar in consistency.
He's primarily breastfed, but we're gonna try and introduce the Bamba now, today, in graduated amounts and prove that he doesn't react to it, and if that's the case, then we're gonna encourage Mom, LaRetta, to continue exposure and feeding of Bamba at least three times a week from now until quite a while from now.
LaRetta: You know, asthma kills and so do allergies, and so you just, I don't necessarily worry.
I just wanna be on top of it.
There's worse things in life, but it can kill.
Travis: We wanna make sure that we're doing this in the doctor's office.
That's one of the things that we wanna make sure.
LaRetta: Oh, you gotta put your hand down.
Oh, yum, yum, yum.
Travis: And it's recommended that you do it under the guidance of an allergist, because if there is an allergic reaction, they can be-- "That was kind of a lot, how you doing?"
They can be significant.
"Ready for some more, Mister?"
Travis: Should we go up, wanna do the same thing?
I'll hold him.
Sure.
Narrator: Garrett does great with the Bamba challenge.
Travis: But this will allow Garrett to live healthy in a world with peanuts.
♪♪ Joanne: The other thing that's out there has been a peanut patch.
We've talked to Danielle about these options.
She hasn't undertaken any of 'em at this time.
"Natalie..." Joanne: Right after Natalie's passing, it was, I think, for any of us to psychologically get our heads around trying to do it, nobody was in the right place.
Narrator: The peanut patch is cutting edge.
Travis: It's a patch that's very similar to the nicotine patch that we're familiar with.
So for somebody maybe like Danielle, where you're not ready to ingest and be in a very intense treatment program, the patch will offer a really nice option to start moving the immune system in the right direction.
Narrator: As new treatments are developed, food allergies are impacting schools everywhere.
(girl laughing) Angie Richter: I've been a school nurse for 12 years, and I definitely see an increase, In the number of epi pens I have at my middle school right now is, I'd say, doubled.
Narrator: Angie Richter works for the San Juan School District.
Angie: First of all, we identify our students, and that's usually by the emergency card or a parent reports to us that their child has a food allergy.
Then the nurses write an individualized care plan for that student based on his food allergies.
The care plan's given to the teacher.
We obtain epi pen auto-injectors.
Our cafeterias are peanut-free.
We don't serve any peanut products on our campuses.
Some of the administrators offer peanut-free tables in their schools, and those children with food allergies may sit at them and feel like they have a safe place at lunchtime to eat.
Narrator: At Camellia Waldorf private school, administrators recently voted to make the entire campus peanut-free out of concern for students' peanut allergies.
Laura Embrey: We have a student here who is terribly allergic to peanuts.
Diego Arteaga: My throat closes up and I can't breathe, so I have to take my epi pen.
Antonio Arteaga: We found out he was allergic to peanuts about the age of 2 1/2.
He has asthma when he gets sick, and so for him, when he was young, it was constant runny nose, constant wheezing.
He spent a week in the hospital, so they suggested we go see an allergist.
Laura: This is very serious.
It causes real illness.
Reya Harmon: I'm allergic to nuts and kiwis and avocados.
Mostly nuts, though.
Well, I know when I eat nuts, my throat starts to swell, and I have a epi pen, so we have to use that, but it has never happened to me, so we've never had to use it.
Narrator: Teachers have epi pens on campus.
Laura: To parents, I would say communicate with the teacher.
Communicate, communicate, communicate.
Narrator: In addition to food allergies, many kids today are also experiencing food intolerances.
Rubina: An intolerance can be something where it's not necessarily your immune system overreacting but that you don't digest this food very well or that it has some side effects that are common.
Pierce Stinson: I have a food sensitivity to dairy.
Narrator: Food allergies are sometimes confused with a food sensitivity or intolerance.
A true food allergy impacts the immune system and can be life threatening.
Food intolerance is an absence of an enzyme needed to fully digest a food.
Pierce: It just makes me phlegmy, sometimes out of control.
My mind gets all, like, kinda just go crazy.
NARRATOR: 10-year-old Levi Woods loves jumping rope, going to school, and knows to stay away from foods containing red dye, candies, toothpaste, anything red.
Levi Woods: When I eat red dye, I get really emotional.
I get really mad and sad.
Pierce: I've never really needed an epi pen.
Again, it's not really life threatening.
Victoria: You eat a food, you note reactivity to that food.
And if you can eat a food and consistently note the same reactivity to that food, then yes, clearly those are linked.
And if it doesn't make you feel good, then don't eat it.
Narrator: We also hear a lot these days about gluten and wheat.
Celiac disease is an immune-system-based reaction but is not considered a food allergy.
Rubina: That's a little different from gluten sensitivity, which is actually a very well-described entity now, where there are a number of people who are sensitive to an actual sugar molecule on top of the gluten.
And what that does is it makes them have very significant bloating, abdominal pain, and cramping.
Narrator: Celiac disease, sensitivities, allergies, it's all food for thought.
Joanne: I just want people to know that Natalie, first and foremost, would want people to know her story and to hope that her story makes something easier for the next young person.
Narrator: The Giorgi family left Carmichael after their daughter died.
They moved back home to the Bay Area to be near family.
Danielle: We're at the cemetery at Natalie's bench.
Narrator: The Giorgi family took us to where Natalie is buried the day before the twins' birthday.
Joanne: Tomorrow's Natalie and Danielle's birthday, and so, you know, Natalie, we try and mark the day for both girls and make it special, so for Natalie, we will take her out her birthday balloon and some fresh flowers.
♪♪ Narrator: Danielle turns 19, but forever, her identical twin sister, Natalie, will be 13.
Danielle: It's weird 'cause, you know, you're celebrating her, but you don't really see her and, I don't know.
Michael: It still really gets me down all the time.
I miss my sister dearly.
Narrator: Since the move to the Bay Area, Danielle now receives treatment for her allergies from Stanford.
Travis: I was honored to help them.
Narrator: Dr. Miller still stays in touch.
Travis: With identical twins, there's probably a shared soul, in some sense, and it would make it more intense.
Narrator: The grieving is not going away, but the Giorgis want Natalie's young life to make a difference.
I think that the family has also taken this opportunity to turn around and make themselves advocates for the food allergy community, and I think that's a wonderful way to help protect others by education and by empowerment.
Catherine: If her passing away had to save all these other kids, then I guess I'm proud of her then (laughs), even though it wasn't her doing.
She didn't wanna pass away so young, she's helping a lot of other kids.
Joanne: Natalie, she had such a beautiful spirit.
Her ability to actually understand the challenges of others was extraordinary in a 13-year-old.
♪♪ Narrator: Appropriately, this year for her birthday, through her family sharing her story, Natalie is giving back to the world.
Joanne: I think if I had to summarize her, she would say, let these lessons of what happened to me help make it easier for another child.
Natalie's nickname was the Sunshine Girl.
Narrator: Always and forever, the Sunshine Girl will be a ray of light and hope.
Announcer: This ViewFinder episode is supported by UC Davis Health, where doctors, nurses, and researchers share a passion for advancing health.
Learn more about their latest medical innovations at health.ucdavis.edu.
♪♪ ♪♪
Support for PBS provided by:
ViewFinder is a local public television program presented by KVIE
Series sponsored by SAFE Credit Union. Episode sponsored by UC Davis Health.